How technology can help tackle increasing demands on healthcare?
In the USA, as in the other parts of the world, population growth increased longevity, and more chronic conditions are increasing its healthcare challenges. National health expenditure grew 4.6% to $3.6 trillion in 2018, or $11,172 per person, and accounted for 17.7% of Gross Domestic Product (GDP). At the time of constrained health and social care budgets, Medicare spending grew 6.4% to $750.2 billion in 2018 or 21 percent of total NHE.
The challenge for the future sustainability of healthcare systems is to find a balance between
- Constrained budgets and the rising cost of advanced medical treatments.
- Increasing complexity and costs delivering care to an aging population.
- Increasing patient expectations and demand for better quality, patient-centered healthcare.
- Reduced availability and increased costs of health care providers, in-patient beds, and residential care.
1. Rise of mHealth or on-demand healthcare services
More than four billion people globally are on the Internet and you can start to see the possibilities that digital transformation in healthcare offers. Smartphone owners are being encouraged to exercise, lose weight and improve the monitoring of their health via an astounding number of mobile applications.
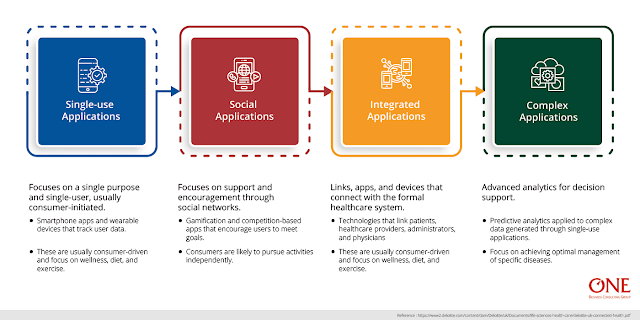
Digital and mobile health applications range from simple to complex mobile applications:
- Single-use Applications: Focuses on a single purpose and single-user, usually consumer-initiated. Eg: Smartphone apps and wearable devices that track user data. These are usually consumer-driven and focus on wellness, diet, and exercise.
- Social Applications: Focuses on support and encouragement through social networks. Eg: Gamification and competition-based apps that encourage users to meet goals. Consumers are likely to pursue activities independently.
- Integrated Application: Links, apps, and devices that connect with the formal healthcare system. Eg: technologies that link patients, healthcare providers, administrators, and physicians. Custom made to multiple end-users: Patients, healthcare providers, and administrators.
- Complex applications: Advanced analytics for decision support. Predictive analytics applied to complex data generated through single-use applications. Focus on achieving optimal management of specific diseases.
A report based on research by the IMS Institute of healthcare informatics examined over 43000 mobile health applications that were available for download in Android and Apple phones. The research found that only 23,682 had a legitimate health function, 7,407 were aimed at Health care professionals, 16,275 were aimed at patients/direct consumers.
2. Wearable devices
Another key development is the growth in wearable technology, and in particular, biosensing wearables. These devices include fitness bands, digital hearing aids, blood pressure monitors, and ingestible devices such as smart pills. Most of the healthcare devices transmit data via an app.
There are 3 main characteristics impacting the wearables.
- Wearables work well only in conjunction with software (apps)
- There is a demand for monitoring devices that are unobtrusive and easy to use.
- The market of wearable devices is highly fragmented and there are many small companies manufacturing it.
Benefits for healthcare companies who invest in these products:
- Personalizes the healthcare experience – medical devices give patients a sense of ownership in the process of improving their health.
- Target's insurance pricing – information obtained from wearable devices can help insurers more accurately rate a patient’s risk for illness.
- Provides insurance incentives – patients who take preventive measures to improve their health can obtain lower insurance premiums.
- Provides gamification opportunities – some medical devices such as fitness watches can create competitive goals for users to achieve through exercise, diet, and nutrition.
3. The importance of Big data in healthcare
As the need for good and affordable healthcare mounts, using data to make better-informed healthcare decisions is essential. By deploying artificial intelligence (AI), healthcare organizations can leverage vast troves of data to better anticipate patient needs, staff for them, improve treatment decisions, and reduce health risks in select cohorts.
- Analytics is the ability to record and playback information. You can record the diagnoses for each patient and report on how many have a particular illness.
- Analytics becomes advanced analytics when you write algorithms to search for hidden patterns. You can cluster patients based on similar symptoms.
- Machine learning is when the algorithm gets better with experience. The algorithm learns, from examples, to predict the onset of illness.
- AI is when a machine performs a task that human beings find interesting, useful and difficult to do. Your system is artificially intelligent if, for example, machine-learning algorithms predict the outbreak of illness in a community and construct an outreach plan.
How to make sense of Analytics in Healthcare?
- Analytics: Report number of patients with illness
- Advanced Analytics: Cluster patients with similar symptoms
- Machine Learning: Predict the onset of an illness
- Artificial Intelligence: Detect the risk of illness and recommend a community outreach plan
Here’s what it looks like when you apply industrialized AI in healthcare.
- Be more efficient: Hospitals have the potential to reduce expenditures by 8 percent. We can increase the efficiency of care by anticipating patient needs and responding accordingly.
- Be more responsive: 60 to 70 percent of hospital costs come from staff labor. AI can increase the effectiveness of hospital staff and save $200 for every patient treated.
- Be more effective: Personalized care can add a year to the life expectancy of patients. AI helps personalize medicine by automatically intervening on behalf of the patient.
4. Connected providers: transforming ways of working
The exponential rise in technology-enabled care requires healthcare providers to redefine staff roles and responsibilities and enable them to work differently. Currently, healthcare is largely defined by “place” of work and based on providing hands-on care to patients. As technology is adopted, staff can undertake e-visits, write e-prescriptions and track, diagnose and deliver treatment via remote digital monitoring, delivering benefits for providers, with savings in cost and time.
- Improving healthcare in residential and nursing homes: 4.5 percent (about 1.5 million) of older adults live in nursing homes and 2 percent (1 million) in assisted living facilities. The majority of older adults (93.5 percent, or 33.4 million) live in the community. Care home residents have 40 to 50 percent more emergencies. 42% of the adults in care homes are in the last six months of life.
- Supporting care at home: Mobile technology has huge potential to help NHS organizations deliver more effective home care and support re-enablement. For instance, 24/7 remote monitoring can facilitate earlier discharge and reduce hospital admissions.
- Improve the efficiency of care: Community services provide health, well being and care from childhood to end of life. Community services can help move more services out of hospitals, closer to home, and shift the focus from reactive care to preventive care. Designing community services in a way that connects them to the rest of the health and social care system requires fully integrated mobile solutions and a technology platform that provides healthcare professionals with a consistent user interface to the information they need. Indeed community healthcare workers require a user interface that can work both online and offline.
- Transforming hospital care: Digital capability in hospitals is variable, with most hospitals having a large number of separate and unconnected systems. The US is leading the way in using digital technology and telemedicine to transform ways of working across hospitals and community care.
Conclusion:
Connected health seeks to improve people’s ability to self-manage their health and well being, alert healthcare professionals to changes in their condition and support medication adherence. For health and social care providers, it can help deliver safer, more efficient and cost-effective care.
The task at hand for healthcare providers, commissioners, and payers across the world is to adopt technology at scale and we, at ONE BCG hope to support in doing so. As ever, welcome your feedback and suggestions.
References:
https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nhe-fact-sheet
https://www2.deloitte.com/content/dam/Deloitte/uk/Documents/life-sciences-health-care/deloitte-uk-connected-health.pdf
https://www.mckinsey.com/business-functions/mckinsey-digital/our-insights/big-data-the-next-frontier-for-innovation





No comments: